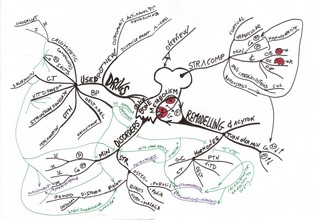
Bone (Rang)
Structure & Composition (Rang)
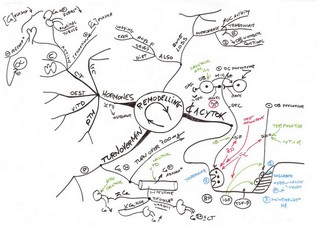
Remodelling (Rang)
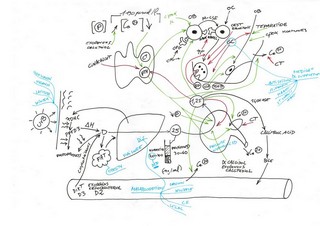
Vitamin D (Moi)
| ANXIOLYTICS & HYPNOTICS/SEDATIVES Anxiety disorders : Increased NE; decreased GABA and serotonin |
| (Neal Glance 9e 2020) V1 JPG |
| Barbiturates Ultra-short action (thiopental) Short action (seco-barbital) Long action (pheno-barbital) Benzodiazepines Short action (tria-zolam) Intermediate action (alpra-zolam) Lora-zepam Long action (flura-zepam) Non BZ Miscellaneous agents Buspirone Chloral hydrate Eszopiclone Ramelteon Zaleplon Zolpidem Insomnia therapy Triptans |
| CLINICALLY IMPORTANT ALCOHOLS & THEIR ANTAGONISTS |
| EPILEPSY/SEIZURES |
| (Neal Glance 9e 2020) V1 JPG |
| Epilepsy therapy Tonic-clonic & partial seizures Absence seizures Myoclonic seizures Back-up & adjunctive drugs |
| Neurodegenerative disease therapy Alzheimer disease Amyotrophic lateral sclerosis Huntington disease PARKINSON Parkinson’s disease : Decreased dopamine |
| (Neal Glance 9e 2020) V1 JPG |
| Parkinsonism disease therapy Carbidopa/levodopa Other movement disorders |
| ALZHEIMER Alzheimer’s disease : Decreased acetylcholine Huntington’s disease : Decreased GABA & acetylcholine |
| Acetylcholinesterase inhibitors N-methyl-D-aspartate (NMDA)-receptor antagonist Memantine |
| PSYCHOSES & BIPOLAR LITHIUM Schizophrenia : Increased dopamine |
| (Neal Glance 9e 2020) V1 JPG |
| ANTIPSYCHOTICS Typical Classic drugs (D2 receptor affinity) Haloperidol Atypical Newer agents (5HT2 receptor affinity) Queti-apine -idone BIPOLAR Classic drug Lithium Newer agents carbamazepine clonazepam olanzapine valproic acid others |
| ANTIDEPRESSANTS Depression : Decreased NE & serotonin |
| (Neal Glance 9e 2020) V1 JPG |
| Antidepressants Selective Serotonin Reuptake Inhibitors (escitalopram, fluoxetine, fluvoxamine, paroxetine, sertraline) Serotonin-Norepinephrine Reuptake Inhibitors (duloxetine, venlafaxine) Tricyclic Antidepressants (ami-triptyline, clom-ipramine, im-ipramine) Monoamine Oxidase Inhibitors (phenelzine, selegiline, tranylcypromine) Atypical Heterocyclic Tetracyclic (amoxapine, bupropion,mirtazapine (tetra)) 5HT2 R Antagonists (nefazodone, trazodone) DNRI Bupropion |
| OPIOID ANALGESICS & ANTAGONISTS |
| (Neal Glance 9e 2020) V1 JPG |
| Opioid analgesics Tramadol Mixed agonist and antagonist opioid analgesics Capsaicin Opioid detoxification and relapse prevention |
| DRUG ABUSE |
| (Neal Glance 9e 2020 Drug abuse) V1 JPG |
| RENAL |
|
(Neal Glance 9e 2020) V1 JPG (Lerchenfeldt BRS 7e 2019 Contents) V1 PDF |
| DIURETICS/DRUGS THAT MODIFY SALT EXCRETION Site of action PCT Carbonic anhydrase inhibitors (acetazolamide) TAL Loop diuretics (furosemide) DCT Thiazides (hydrochlorothiazide) CCT K+-sparing diuretics (spironolactone) Osmotic diuretics (mannitol) Electrolyte changes Angiotensin-converting enzyme inhibitors Angiotensin II receptor blockers Aliskiren ANTIDIURETIC/DRUGS THAT MODIFY WATER EXCRETION Mannitol ADH agonists (desmopressin) ADH antagonists (conivaptan) |
| CARDIOVASCULAR |
|
(Neal Glance 9e 2020) V1 JPG HT 1 Angina 2 Antiarr 3 HF 4 (Lerchenfeldt BRS 7e 2019 Contents) V1 PDF |
| HYPERTENSION |
| Hypertension treatment Cardiovascular agents & molecular targets Emergency Diuretics Sympathoplegics—blockers of CNS sympathetic outflow (Clonidine) Ganglia (Hexamethonium) Nerve terminals (Guanethidine, Reserpine) Alpha or beta receptors (Prazosin, Propranolol) Vasodilators Older oral vasodilators (Hydralazine) Calcium channel blockers (Nifedipine) Parenteral vasodilators (Nitroprusside) Angiotensin antagonists ACE inhibitors (Captopril) Receptor blockers (Losartan) Renin inhibitor (Aliskiren) |
| ANGINA PECTORIS |
| Antianginal therapy Ranolazine Sacubitril Vasodilators Nitrates Short duration (sublingual nitroglycerin) Intermediate (oral nitroglycerin) Long duration (transdermal nitroglycerin) Vasodilators Calcium blockers (verapamil) Cardiac depressants Calcium blockers (verapamil) Cardiac depressants Beta blockers (propranolol) Other drugs Metabolism modifiers; rate inhibitors |
| HEART FAILURE |
| Positive inotropic drugs Cardiac glycosides (digoxin) Beta agonists (dobutamine) PDE inhibitors (milrinone) Vasodilators Vasodilators Nitroprusside nitrates hydralazine Loop diuretics, angiotensin inhibitors, nesiritide, sacubitril, SGLT2 inhibitors Miscellaneous drugs for chronic failure Beta blockers, spironolactone |
| ARRHYTHMIAS |
| Group 1 Sodium channel blockers (procainamide) Group 2 β blockers (esmolol) Group 3 Potassium channel blockers (amiodarone,dofetilide) Group 4 Calcium channel blockers (verapamil) Group 5 Miscellaneous group (adenosine, K+, Mg2+) Ivabradine |
| VASCULAR |
| GASTROINTESTINAL |
|
(Neal Glance 9e 2020) V1 JPG PU 1 Motility & Secretions 2 (Lerchenfeldt BRS 7e 2019 Contents) V1 PDF |
| ANTIEMETIC/NAUSEA & VERTIGO |
| (Neal Glance 9e 2020) V1 JPG |
| Benzodiazepine (Lorazepam) Selective 5-HT3 blockers (ondansetron) D2 blockers (prochlorperazine) H1 blockers (diphenhydramine) Antimuscarinics M1 (scopolamine) Corticosteroids (dexamethasone) Cannabinoids (dronabinol) Neurokinin receptor 1 antagonists (aprepitant) |
| OBESITY |
| GLP 1 R Ago Lipase I 5-HT agonist (lorcaserin) Amphetamine-mimetics (phentermine) Symp Miscellaneous |
| TO INCREASE APPETITE Megestrol Dronabinol |
| ACID-PEPTIC ULCER |
| Acid suppression therapy Antacids (Mg[OH]2), CaCO3 H2-blockers (cimetidine) Proton pump inhibitors (omeprazole) Mucosal protective agents (sucralfate, misoprostol, bismuth compounds) Antibiotics |
| OTHER |
|
Constipation Bulk-forming laxatives Irritant (stimulant) laxatives (cathartics) Lubricating agent Osmotic laxatives Opoid R antago Stool softener Diarrhea Flatulence Motility promoters Prokinetic Metoclopramide, cholinomimetics Drugs for irritable bowel syndrome IBS Anticholinergics, serotonin antagonists Drugs for inflammatory bowel disease IBD 5-ASA drugs, corticosteroids immunosuppressants, anti-TNF drugs Other agents Pancreatic lipase, laxatives, antidiarrheals ursodiol Octreotide Sulfasalazine Loperamide Orlistat |
| PULMONARY |
|
(Neal Glance 9e 2020) V1 JPG (Lerchenfeldt BRS 7e 2019 Contents) V1 PDF |
| ASTHMA & OTHER BRONCHIAL Bronchodilators COPD Beta2 agonists : SABAs LABAs Muscarinic antagonists Methylxanthines Anti-inflammatory agents Release inhibitors Steroids Ihn GC COPD Slow anti-inflammatory drugs Antibodies Leukotriene antagonists Is Lipoxygenase inhibitors Receptor inhibitors PDE4 Inh Anti-IgE Ab RHINITIS Anti H1 H1-blockers Alpha ago COUGH Antitussives Expectorants Mucolytics Chromones Dextromethorphan Pseudoephedrine, phenylephrine CHRONIC OBSTRUCTIVE PULMONARY DISEASE Antibiotics PULMONARY HYPERTENSION |
| ENDOCRINE (Lerchenfeldt BRS 7e 2019 Contents) V1 PDF |
| HYPOTHALAMIC/PITUITARY DRUGS |
| HYPOTHALAMUS GnRH Agonist action Gonadorelin Antagonist action GnRH receptor agonist (leuprolide) GnRH receptor antagonist (ganirelix) ANTERIOR PITUITARY Growth hormone Agonist action Somatropin Mecasermin Antagonist action Octreotide Pegvisomant Gonadotropins Agonist action Mixed LH & FSH Menotropins LH Lutropin hCG FSH Follitropin Prolactin Antagonist action D2 dopamine agonists (bromocriptine) POSTERIOR PITUITARY Oxytocin Agonist action Oxytocin Antagonist action Atosiban (not FDA approved) Vasopressin Agonist action Desmopressin Antagonist action Conivaptan |
| CORTICOSTEROIDS |
| (Neal Glance 9e 2020) V1 JPG |
| Agonists Glucocorticoids (prednisone) Mineralocorticoids (fludrocortisone) Antagonists Receptor antagonists Glucocorticoid antagonists (mifepristone) Mineralocorticoid antagonists (spironolactone) Synthesis inhibitors (ketoconazole) Cinacalcet Sevelamer Cation exchange resins |
| REPRODUCTIVE |
| (Neal Glance 9e 2020) V1 JPG |
| Estrogens (ethinyl estradiol) Antiestrogens Receptor antagonists Full antagonists (fulvestrant) SERMs (tamoxifen) Aromatase inhibitors (anastrozole) Other (GnRH agonists, danazol) Progestins (L-norgestrel) R modulator ? Ulipristal acetate ? Antiprogestins (mifepristone) Androgens (testosterone) methyltestosterone Antiandrogens Receptor antagonists (flutamide) 5α-Reductase inhibitors (finasteride) Synthesis inhibitors (ketoconazole) Other (GnRH agonist, combined oral contraceptives) Control of reproductive hormones Degarelix Hormone replacement therapy Combined contraception Copper intrauterine device Tocolytics Danazol Tamsulosin Minoxidil |
| THYROID |
| (Neal Glance 9e 2020) V1 JPG |
| Hypothyroidism Levothyroxine (T4) Liothyronine (T3) Hyperthyroidism Thioamides (propythiouracil) Iodide (Lugol solution) Beta blockers (propranolol) 131I |
| DIABETES MELLITUS |
| (Neal Glance 9e 2020) V1 JPG |
| Diabetes mellitus therapy Insulins Ultra short Rapid, short-acting (lispro, regular) Intermediate-acting (NPH, lente) Slow, long-acting (glargine) Ultra long Noninsulin antidiabetic drugs Insulin secretagogues (glipizide) sulfonylureas Meglitinides ? Biguanides (metformin) Alpha-glucosidase inhibitors (acarbose) Thiazolidinediones (pioglitazone) Amylin analogs (pramlintide) Incretin modulators GLP-1 analog (exenatide) DPP-4 inhibitor (sitagliptin) SGLT2 inhibitors (canagliflozin) Increase blood glucose Diazoxide Glucagon |
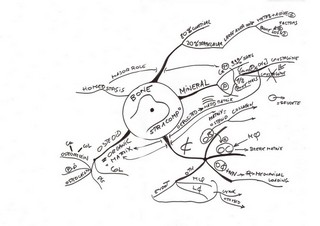
| BONE MINERAL HOMEOSTASIS |
| Hormonal PTH Vitamin D Calcitonin Estrogen Glucocorticoids Nonhormonal Bisphosphonates Fluoride Calcimimetics |
| RETINOIC ACID DERIVATIVES |
| AUTACOIDS, ERGOTS & ANTI-INFLAMMATORY (Lerchenfeldt BRS 7e 2019 Contents) V1 PDF |
| Kinins Kininogen (HMWK, LMWK) Bradykinin Kallidin Tachykinins Urotensin-II Others Angiotensin Eicosanoid Histamine Platelet-activating factor Serotonin Palmitoylethanolamide |
| HISTAMINE RECEPTOR BLOCKERS |
| H1 blockers -tadine First generation (diphenhydramine) Second generation (cetirizine) H2 blockers (cime-tidine) |
| SEROTONIN RECEPTOR AGONISTS AND ANTAGONISTS |
| Agonists, partial agonists 5-HT1 agonists (sumatriptan) 5-HT4 partial agonists (tegaserod) Antagonists 5-HT2 antagonists (ketanserin) 5-HT3 antagonists (ondansetron) |
| ERGOT ALKALOIDS |
| VASOACTIVE PEPTIDES Vasoconstrictors (angiotensin II, endothelins, neuropeptide Y) Mixed (substance P) Vasodilators (bradykinin, BNP, ANP,CGRP, VIP) |
| Antagonists of peptides Renin (aliskiren) ACE (captopril) Angiotensin (losartan) Vasopressin (conivaptan) Endothelin (bosentan) Vasopeptidase (omapatrilat) Substance P (aprepitant) |
| EICOSANOIDS |
| Arachidonic acid pathways Leukotrienes (LTB4, LTC4, LTD4) Prostaglandins (PGE1, PGE2, PGF2), Prostacyclin (PGI2), Thromboxane (TXA2) Eicosanoid antagonists Leukotriene antagonists (zileuton, montelukast, zafirlukast) Prostaglandin antagonists (corticosteroids, NSAIDs) |
| NITRIC OXIDE |
| NSAIDS, ACETAMINOPHEN, & RHEUMATOID ARTHRITIS & GOUT |
| (Neal Glance 9e 2020) V1 JPG |
| ANTI-INFLAMMATORY NSAIDs Aspirin Other nonselective NSAIDs COX-2 inhibitors (celecoxib) DMARDs Conventional synthetic (cs) DMARDS Biologic (b) DMARDS ACETAMINOPHEN GOUT Acute NSAIDs Glucocorticoids Chronic Colchicine Uricosurics (probenecid) Xanthine oxidase inhibitors (allopurinol, febuxostat) Leflunomide Bisphosphonates Teriparatide TNF-α inhibitors Imiquimod |
| ANEMIA & HEMOSTASIS & LIPIDS |
|
(Neal Glance 9e 2020) V1 JPG Coag 1 Lip 2 Anem 3 (Lerchenfeldt BRS 7e 2019 Contents) V1 PDF |
| LIPIDS-LOWERING HMG-CoA reductase inhibitors (lovastatin) Resins Ezetimibe Niacin Fibrates (gemfibrozil) PCSK9 Inhibitors (alirocumab, evocumab) |
| HEMATOPOIETIC FACTORS |
| Erythrocyte factors Vitamins (B12, folate) Iron Erythropoiesis-stimulating agents (ESAs; erythropoietin) Platelet factor Oprelvekin (IL-11) Granulocyte factors Filgrastim (G-CSF) Sargramostim (GM-CSF) |
| COAGULATION/CLOTTING |
| ANTICLOTTING Anticoagulants Heparins Direct thrombin inhibitors Direct factor Xa inhibitors Warfarin Heparin vs warfarin Direct coagulation factor inhibitors Anticoagulation reversal Thrombolytics t-PA derivatives Streptokinase Antiplatelet drugs Aspirin Glycoprotein IIb/IIla inhibitors ADP inhibitors (clopidogrel) PDE/adenosine uptake inhibitors FACILITATE CLOTTING Replacement factors Vitamin K Antiplasmin drugs |
| ANTIMICROBIAL |
| ANTIBACTERIAL |
|
(Neal Glance 9e 2020) V1 JPG NA 1 CW 2 Prot 3 (Lerchenfeldt BRS 7e 2019 Contents) V1 PDF |
| ANTIMICROBIAL THERAPY CELL WALL SYNTHESIS INHIBITORS Penicillins Narrow spectrum : Penicillinase-sensitive, Penicillinase-resistant Wider spectrum Prototype G V, G benzathine and G procaine Penicillinase-resistant Extended-spectrum Beta·Lactamase inhibitors Antipseudomonal Piperacillin -cillin Transpeptidase inhibitor Ampicillin Cephalosporins Narrow spectrum 1st generation Wider spectrum 2nd, 3rd, 4th generations 5th generation Combinations Carbapenems Monobactam Aztreonam Glycopeptides Vancomycin Lipopeptide Daptomycin Other PROTEIN SYNTHESIS INHIBITORS Broad spectrum Chloramphenicol Tetra-cycline-s Protein synthesis inhibitor Moderate spectrum Macrolides -thromycin Ketolide Narrow spectrum Lincosamides Clindamycin Streptogramins Quinupristin plus dalfopristin Oxazolidinones Linezolid AMINOGLYCOSIDES 30S & SPECTINO-MYCIN Glycylcline Tigecycline SULFONAMIDES, TRIMETHOPRIM, & FLUOROQUINOLONES Antimetabolites Antifolates Sulfonamides Trimethoprim Trimethoprim-sulfamethoxazole Pyrimethamine Fluoroquinolones Narrow spectrum 1st generation (eg, nor-floxacin) Wide spectrum 2nd generation (eg, ciprofloxacin) 3rd generation (eg, levofloxacin) Miscellaneous inhibitors of bacterial nucleic acid synthesis Metrodinazole Nitrofurantoin Miscellaneous Mupirocin Polymixin B ANTIMYCOBACTERIAL Drugs used in tuberculosis First-line drugs (isoniazid, rifampin, ethambutol, pyrazinamide, streptomycin) Alternative drugs (amikacin, ciprofloxacin, ethionamide, p-aminosalicylate) Drugs used in leprosy Acedapsone, dapsone, clofazimine, rifampin Drugs used for nontuberculous mycobacteria Azithromycin, clarithromycin, moxifloxacin Tigecycline Clindamycin Linezolid Daptomycin Rifamycins ANTIMICROBIAL PROPHYLAXIS PROPHYLAXIS IN HIV INFECTION/AIDS |
| ANTIFUNGAL |
| (Neal Glance 9e 2020) V1 JPG |
| ANTIFUNGAL THERAPY DRUGS ACTING ON FUNGI Alter cell membrane permeability Azoles Polyenes Terbinafine -conazole Ergosterol synthesis inhibitor Ketoconazole Block beta-glucan synthesis Echinocandins Block nucleic acid synthesis Flucytosine Disrupt microtubule functions Griseofulvin Amphotericin B Nystatin |
| ANTIVIRAL |
| (Neal Glance 9e 2020) V1 JPG |
| ANTIHELMINTH |
|
(Neal Glance 9e 2020) V1 JPG |
| Antihelminthic therapy ANTIHELMINTHIC DRUGS Drugs active against nematodes Albendazole Diethylcarbamazine Ivermectin Mebendazole Pyrantel pamoate Drugs active against trematodes Bithionol Metrifonate Oxamniquine Praziquantel Drugs active against cestodes Al-bendazole Mebendazole Niclosamide Praziquantel |
| ANTIPROTOZOAL |
| (Neal Glance 9e 2020) V1 JPG |
| Antiprotozoal therapy ANTIPROTOZOAL DRUGS Antimalarial agents Chloroquine Artemisinins Mefloquine Primaquine Quinine Antifolates Others Drugs for amebiasis Metronidazole Diloxanide Emetine Iodoquinol Drugs used for other parasites Pneumocystosis Toxoplasmosis Leishmaniasis Trypanosomiasis Anti-mite/louse therapy |
| CANCER |
|
(Neal Glance 9e 2020) V1 JPG (Lerchenfeldt BRS 7e 2019 Contents) V1 PDF |
|
Cancer therapy—cell cycle Cancer therapy—targets Alkylating agents Nitrogen mustards Cyclophosphamide Alkyl sulfonate Nitrosoureas car-mustine Platinum analogs compounds Cis-platin Proteasome inhibitors Borte-zom-ib carfilzomib Antimetabolites 5-Fluorouracil, methotrexate, gemcitabine, 6-mercaptopurine Natural products Etoposide Microtubule inhibitors damaging agents Taxanes Pacli-taxel, Microtubule inhibitors damaging agents Vinka alkaloids Vincristine Topoisomerase inhibitors I Irino-tecan II Eto-poside Antitumor antibiotics Bleomycin, Anthracycline Doxo-rubicin mitomycin Miscellaneous Hydroxyurea L-Asparaginase Bortezomib Tretinoin Hormonal Prednisone, tamoxifen Miscellaneous 2 Imatinib Cetuximab Antibody-drug conjugates Monoclonal antibodies Tyrosine kinase inhibitors Immumomodulators small molecule inhibitors Chemotoxicity amelioration Key chemotoxicities |
| IMMUNOLOGICAL |
| (Le FA 1 32e 2022) V1 PDF (From page 19 to page 23) (Neal Glance 9e 2020) V1 JPG |
| Immunosuppressants Corticosteroids (prednisone) Immunophilin ligands (cyclosporine, tacrolimus, sirolimus) Mycophenolate mofetil Cytotoxic drugs (azathioprine) Immunoglobulin based agents (etanercept) Immune potentiators Aldesleukin Interferons |
| BONE |
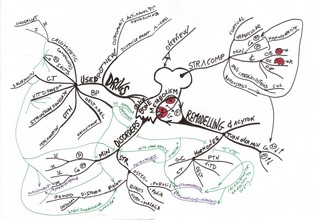 Bone (Rang) | 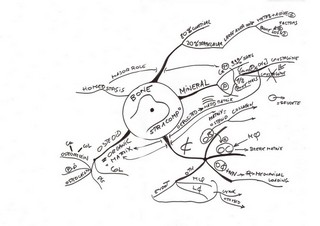 Structure & Composition (Rang) | 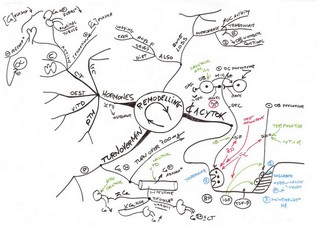 Remodelling (Rang) | 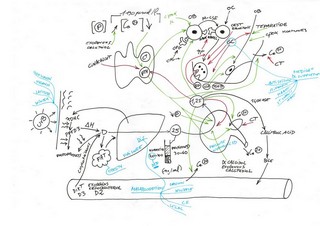 Vitamin D (Moi) |
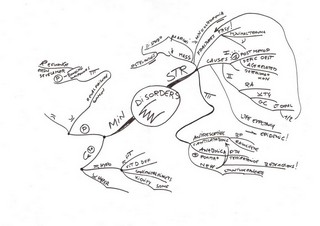 Disorders (Rang) |  Drugs (Rang) |